
The Evolution of the Annual Physical
Traditionally, the annual exam provided clinicians and their patients with a once-yearly snapshot in simple categories: height, weight, blood pressure, basic labs.
The modern longevity exam represents a paradigm shift.
Clinicians can now leverage AI and wearables to up-level their yearly check-ins with patients. These systems give the clinician 365 days of data, instead of the once-a-year touchpoint of a physical and labs.
This shifts care teams to a model of continuous monitoring. The annual appointment becomes a moment of synthesis. Clinicians might use it to review and make suggestions to the patient based on their:
Activity patterns
Glucose levels, including their metabolic response to meals, sleep, and stress
Heart rate variability
Respiratory rate
Symptoms they’ve logged in any applicable apps
Temperature
When clinicians use AI systems to analyze data from the patient’s wearables and self-reporting apps, this gets extra powerful. The annual appointment becomes a moment of reflection and projection.
Much like a company’s annual strategic planning session, it provides a chance to review what’s been learned over the last year of continuous monitoring, then turn that into an actionable plan.
The Role of AI in Making Continuous Care Possible
The explosion of wearable and continuous monitoring data would be clinically unmanageable without AI support. AI platforms:
Filter signal from noise, identifying clinically meaningful patterns in millions of data points
Predict health events (e.g., acute COPD exacerbations, cardiovascular events) based on wearable data patterns
Generate personalized intervention recommendations based on individual response patterns rather than population averages
Free clinician time for high-value patient interaction rather than data review
In short, AI handles pattern recognition at scale. That better positions the clinician to provide clinical oversight, context, and care at the annual appointment and beyond.
Building a Better Longevity Annual Exam
Because the provider has continuous monitoring and AI analysis behind them, they no longer need to use the annual physical to gather and parse data. Instead, they can turn it into an annual health retreat that helps the patient proactively take charge of their wellness.
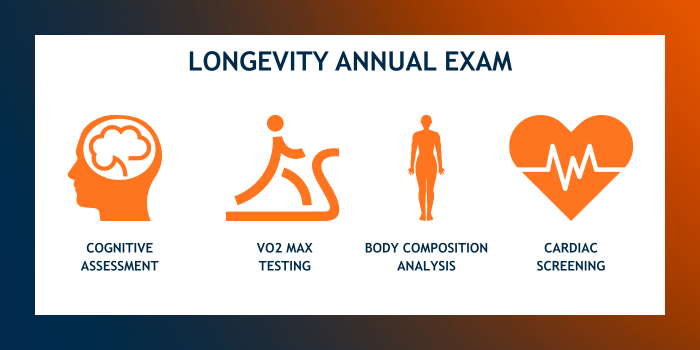
The time previously spent on the basics can be retooled based on the patient’s health wants and needs. The clinician might incorporate:
Body composition analysis: For patients concerned about aging’s effects on bone density, muscle mass, and/or weight.
VO2 max testing: To monitor the patient’s cardiorespiratory fitness, a major predictor of longevity.
Next-level cardiac screening: For patients with a personal or family history of heart issues (e.g., coronary calcium scoring).
Mental health and cognitive assessments: To provide more holistic patient care.
AI enables more sophisticated screenings in many of these areas. AI tools can analyze the person’s facial cues and voice to predict everything from mental health conditions to heart disease, for example.
All of this allows clinicians to address a broader range of well-being markers at the patient’s annual appointment. It goes from a to-do the patient checks off their list to a session they should leave feeling enlightened and empowered around their health.
📙 Your Homework: Applying the Annual Retreat Model at Your Practice
Consider positioning a patient’s upcoming annual exam as an annual wellness retreat. Offer them a strategic health planning session that:
Reviews the past year's continuous data
Updates their biological age
Celebrates wins
Provides an opportunity to request additional testing they want (e.g., VO2 max testing, cognitive function assessment)
Identifies trends and risks
Educates them around their own unique physiology and how interventions are working
Sets goals around their health priorities for the coming year
Gives them a comprehensive report to take home and refer back to
With a clear review of what the year’s health data says about where they are and where they’re going, you provide patients with a roadmap. The information you share during their annual retreat, paired with their take-home report, sets them up to move toward their health goals over the next twelve months.
How I AI with Dr. Jay Parkinson
If you’ve followed the evolution of virtual care, you’ve felt Dr. Jay Parkinson’s fingerprints on it.
A pediatrician by training and one of the earliest pioneers of virtual primary care, Jay spent nearly a decade building Sherpaa’s 24/7 virtual primary care model, and then led clinical design at Crossover Health. He’s been CMO at Nabla and today, he’s the Founder & CEO of Automate Clinic, where he’s exploring the next frontier: how clinicians and AI actually work together in real workflows.
In this conversation, Jay shares why he initially set out to “have doctors train AI models” — and why he’s since shifted focus. His view: it’s still too early (and too expensive) to build healthcare-specific foundation models at scale, but it’s exactly the right time to design AI products that fit how clinicians really practice. Instead of abstract “data labeling,” he imagines workflows that feel like caring for real patients, with AI quietly embedded in the background.
Jay also talks candidly about what it means to be a repeat founder in healthcare: how to build in public, why being wrong in public is a superpower, and why timing and getting more “at-bats” matter more than falling in love with any single idea. On AI, he’s clear that most systems today are more like an 85%-reliable co-pilot — incredibly useful, but only if we design the right human interface and keep clinicians in the loop.
Watch this if you’re a clinician wondering how to lean into AI without losing your judgment, your sanity, or your craft.
Vibrant, the AI-powered Operating System for personalized medicine, can help you transform your annual physicals into wellness retreats by pulling together a full picture of context on your patient with the help of AI. To learn more, schedule some time with our team today.
This Week in Clinical AI
Mayo Clinic launches a global AI-support initiative to help bridge the digital divide. Teams at Mayo Clinic designed Platform_Insights, an extension of the Mayo Clinic Platform, to help healthcare organizations of all sizes. As AI adoption has skyrocketed across the healthcare world, some smaller systems have struggled to keep up. With more than 26 petabytes of clinical information in its network, Platform_Insights aims to connect teams with fewer resources to the latest in AI-driven healthcare tech.
The American Heart Association (AHA) issues new guidance on evaluating AI in cardiovascular care. The AHA acknowledges that AI’s advancement has outstripped the pace of evaluation and guidance. To counter that, the Association proposed four guiding principles that healthcare organizations can use when considering potential AI deployment. The AHA suggests that teams should evaluate tools for strategic alignment, ethics, usefulness/effectiveness, and financial performance.
Hippocratic AI raised $126M at a $3.5B valuation. The generative AI company completed its series C fundraising round, bringing the total of funding it has secured to $404 million. Hippocratic’s AI platform has already been implemented at more than 50 healthcare organizations, including Cleveland Clinic and Northwestern Medicine.
👋 Welcome New Readers
The Modern Clinician is written for functional, integrative, and longevity-focused physicians who want to scale their impact and deliver cutting-edge care.
If you liked this one, share it with a colleague! We appreciate you spreading the word.
To learn more about the why behind this newsletter, start with our first post introducing The Modern Clinician.