
The choice you make here determines whether your clinic thrives or stalls.
We’ve seen it again and again: brilliant clinicians with strong clinical vision, but stuck on the business side.
The ROI of running traditional private practices has been in a state of decline - operating costs have increased while reimbursements have decreased for the last 20 years. That’s why an increasing number of providers are moving away from traditional payor-based models to other business structures.
New business models are emerging as the market for cash pay practices is now growing. But which model is the right one? Picking the wrong model creates constant friction whether that’s unpredictable revenue, admin overload, or a panel size that drains you.
All of this said, there’s no single “best” model. There’s only the one that best aligns with your patients, your lifestyle, and your goals.
The Main Models We See
To help you explore your options, let’s give a quick overview of some of the models we see providers increasingly adopt—and what those models offer:
Membership-based (monthly/annual): Recurring revenue and patient loyalty. Works best when you offer continuous value beyond the visit (e.g., messaging, data review, proactive outreach).
Concierge (high-touch, high-fee): Small panel, white-glove service. Great lifestyle design, but narrows accessibility and requires positioning yourself as ultra-premium.
Direct Primary Care (DPC): Lower monthly fee, bigger panel sizes. Democratizes access, but can drift toward volume-driven care.
Pay-per-visit / Packages: Simple and flexible for patients. Most effective for niche services (hormone consults, IVs, peptide programs) but harder to sustain for comprehensive care.
Insurance or Hybrid: Expands access and volume, but adds administrative burden and reimbursement uncertainty. Can work well if paired with cash-pay programs.
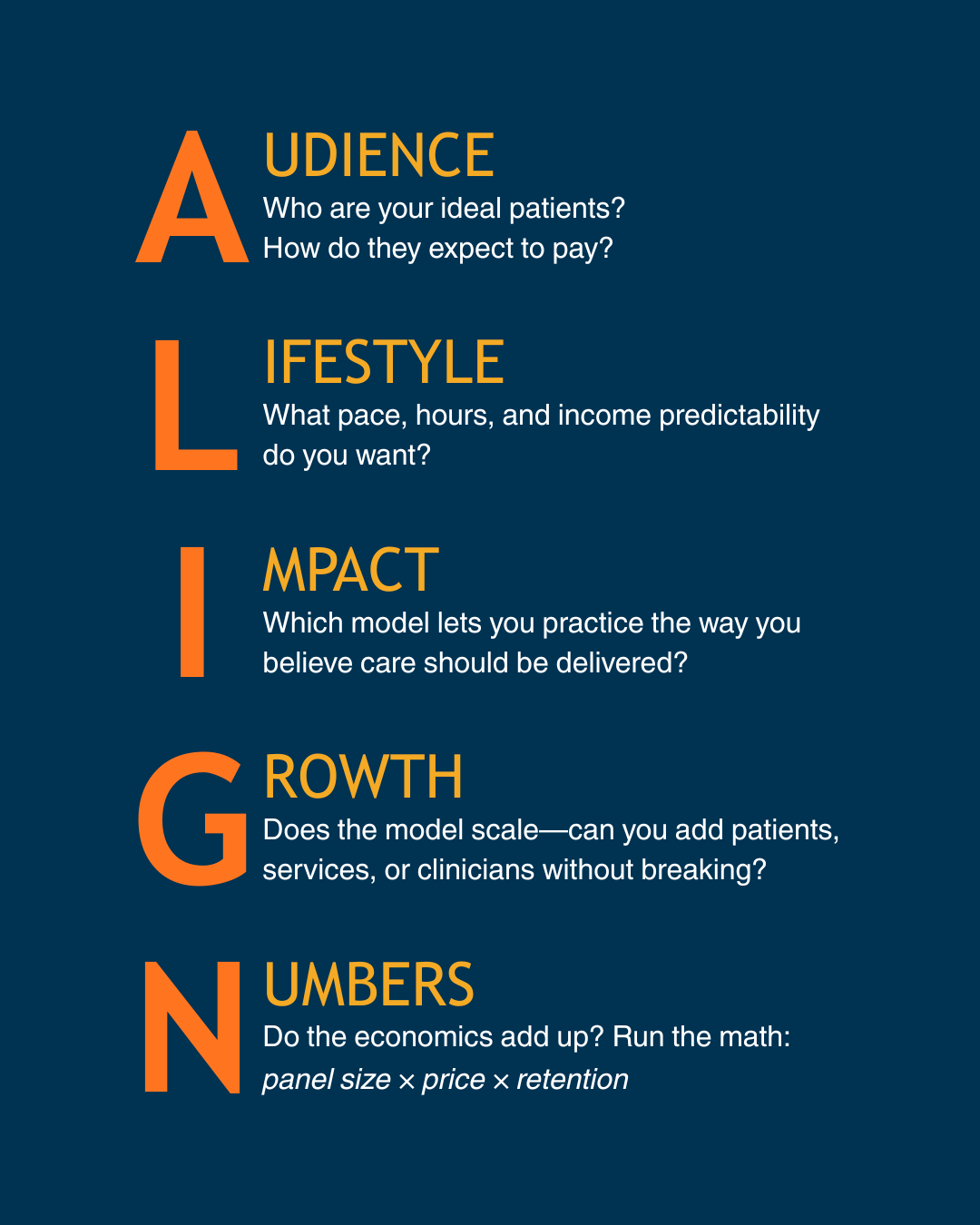
A Simple Framework: ALIGN
Use this lens to pressure-test each option:
Why This Matters
We’ve coached dozens of clinicians through this decision. The ones who succeed long-term are the ones who don’t just pick a model for today—they pick the one that fits their future practice identity.
📙 Try this: Sketch your “ideal week.” How many patients do you see? How much time do you spend on admin? What do you earn? Then run that picture through the ALIGN lens. You’ll quickly see which business model actually supports the life—and impact—you want.
How I AI with Dr. G: Friction Mapping to Enhance the CareSpan Experience
This month’s How I AI spotlights Dr. Lexi Gonzales, Senior Clinical Implementation and AI specialist at OvationLab.
Dr. Gonzalez — or Dr. G — walked us through a simple but powerful way to use ChatGPT’s voice mode: friction mapping your workflows.
Dr. G frames her approach around one question: “Where in my day do things feel harder than they should—for me, my team, or my patients?”
Her process falls into three steps:
Talk it out: Instead of typing, she narrates a workflow aloud—like scheduling a patient, running labs, or sending follow-ups. AI listens for repetition, gaps, and delays that create friction.
Draft the fixes: AI generates a baseline action plan, like merging redundant forms, auto-populating data, or simplifying scheduling. The point isn’t perfection—it’s clarity.
Personalize for practice: Dr. G then adapts the plan for her clinic’s context, weaving in hospitality touches that create the CareSpan Experience—a system where patients feel remembered, respected, and cared for at every touchpoint.
Her philosophy:

📙 Your Homework: Pick one workflow this week: intake, scheduling, or follow-up. Talk it through with ChatGPT voice mode. Capture three friction points and create one small action step to make the process more seamless.
If pre-visit and post-visit workflows are taking a lot of your time, a tool like Vibrant’s our platform can help.
Vibrant’s intelligent operating system means that we hold all the medical records (we are the EHR), but allow you to immediately access all the information in your patient’s chart with the superpowers of AI. No more porting information into ChatGPT and trying to keep it HIPAA compliant. Our secure AI platform can cut down hours worth of prep each week with power AI-native summarization and clinical decision-support.
Our clinicians LOVE saving time with this part of our platform. Interested in trying it out? Get in touch to get started on your own Sandbox environment.
This Week in Clinical AI
AI sees widespread and rapid adoption across medicine. Per the AMA, nearly two-thirds of physicians now use AI. While healthcare is often a change-resistant industry, the fast uptake of AI can be attributed to a pressing need for better tools.
Oldest person passes away, leaving a legacy of new data about lifestyle and genetics. When Maria Branyas Morera passed away in August, she was 117. Happy to contribute to medical research, she provided regular samples of blood, urine, and more. The big takeaway? “It is possible to distinguish molecular changes that happen in the body because of aging from those that occur because of poor health.”
The double-edged sword of hype behind longevity science. Influencers and others promising outcomes from untested treatments have made it harder for scientists to do their jobs. In fact, some longevity researchers now want to rebrand to distance themselves from the movement. Even so, progress advances as we learn more about ways to lead longer, healthier lives.
👋 Welcome New Readers
The Modern Clinician is written for functional, integrative, and longevity-focused physicians who want to scale their impact and deliver cutting-edge care.
If you liked this one, share it with a colleague! We appreciate you spreading the word.
To learn more about the why behind this newsletter, start with our first post introducing The Modern Clinician.